explore
education
tobacco harm reduction
Tobacco harm reduction is a public health strategy to lower the health risks associated with using nicotine.
Smoking tobacco is widely acknowledged as a leading cause of illness and death.
However, nicotine itself is not very harmful, as inferred from the long history of use for nicotine replacement therapy products.
Thus, Tobacco Harm Reduction measures have been focused on reducing or eliminating the use of combustible tobacco by switching to other nicotine products.
nicotine & addiction
Our understanding of nicotine, and addiction itself, is often plagued with misinformation and myths.
smokeless
tobacco
products are not intended to be burned. Made from processed tobacco leaf, they are placed in the mouth
lgbtq
community
suffers disproportionately higher smoking rates, early death, and diseases attributed to smoking
Tobacco Harm Reduction
Harm reduction is a range of practical policies, regulations, actions, and strategies that reduce health risks by providing safer forms of products/substances, or encouraging less risky behaviors.
Harm reduction does not seek to control people, or to prohibit products or behaviors. Harm reduction recognizes the right to engage in risky behavior, but also the right to health – which people never forfeit. When we accept that risky products and behaviors are a part of our society, and we focus our efforts on minimizing harmful outcomes instead of banning, prohibiting, condemning, or stigmatizing, we can effectively improve public health.
Examples of Harm Reduction
- Seatbelts
- Clean Needles
- Helmets
- Condoms
In the course of our lives we all do things or use products that could be dangerous or carry some risk. Many products and activities have been modified to reduce that risk. These modifications can come from product manufacturers, regulators, or be led by consumers. Seatbelts, airbags, and helmets are all examples of harm reduction because they make the act of operating cars and bikes safer. They don’t stop people from driving or riding, and they don’t eliminate all risk, but they save many lives.
Harm reduction is especially important for social justice and human rights, as marginalized communities are often the most affected by misguided policies aimed at prohibiting and eliminating risky behaviors and products, or misinforming the public about real risks. Consider the HIV/AIDS epidemic of the 1980s and the War on Drugs.
Tobacco Harm Reduction (THR) applies the principles of harm reduction to combustible tobacco use (smoking). THR is based on the understanding that people use combustible tobacco for a variety of reasons, and they have the right to do so. THR promotes the use of safer nicotine products for people who want to reduce their risk or stop smoking altogether. Promoting safer products without being coercive, judgemental, or stigmatizing, and ensuring that affected individuals have a voice in the conversation is at the core of THR.
People who smoke have the same fundamental right to health as non-smokers, therefore they deserve the right to access accurate information and products that can help them achieve their health goals.
It is widely understood that quitting the use of all tobacco products achieves the best health outcomes for people who smoke. However, pharmaceutical smoking cessation methods (drugs, gums, patches, etc.) have a 90% failure rate when used as directed. In addition, many people who smoke are unable or unwilling to quit. Harm reduction strategies are more effective and humane than abstinence-only policies.
Harm reduction – specifically THR – is often viewed as a controversial strategy when applied to substance use. Opponents of THR argue that some aspects interfere with cessation and abstinence, and could increase use among young people, despite volumes of research suggesting otherwise.
Knowledge-Action-Change (KAC) (2018). No Fire, No Smoke: The Global State of Tobacco Harm Reduction 2018.
Nitzkin, J (June 2014). “The Case in Favor of E-Cigarettes for Tobacco Harm Reduction”. Int J Environ Res Public Health. 11 (6): 6459–71.doi:10.3390/ijerph110606459. PMC 4078589. PMID 25003176.
Rodu, Brad; Godshall, William T. (2006). “Tobacco harm reduction: An alternative cessation strategy for inveterate smokers”. Harm Reduction Journal. 3: 37. doi:10.1186/1477-7517-3-37. PMC 1779270. PMID 17184539.
Fagerström, KO, Bridgman, K (March 2014). “Tobacco harm reduction: The need for new products that can compete with cigarettes”.Addictive Behaviors. 39 (3): 507–511. doi:10.1016/j.addbeh.2013.11.002. PMID 24290207.
Phillips, CV (November 2009). “Debunking the claim that abstinence is usually healthier for smokers than switching to a low-risk alternative, and other observations about anti-tobacco-harm-reduction arguments”. Harm Reduct. J. 6: 29. doi:10.1186/1477-7517-6-29. PMC 2776004.PMID 19887003.
Sumner W, (2005). “Permissive nicotine regulation as a complement to traditional tobacco control”. BMC Public Health 5:18.
Tomar, SL; Fox, BJ; Severson, HH (2009). “Is smokeless tobacco use an appropriate public health strategy for reducing societal harm from cigarette smoking?”. Int J Environ Res Public Health. 6: 10–24. doi:10.3390/ijerph6010010.
Etter, Jean-François, and John A Stapleton. “Nicotine replacement therapy for long-term smoking cessation: a meta-analysis.” Tobacco control vol. 15,4 (2006): 280-5. doi:10.1136/tc.2005.015487
Nicotine & Addiction
nicotine
It is a common misconception that not much is known about the safety and efficacy of consuming nicotine by non-combustible means. In fact, loads of research was conducted in support of applications to market nicotine replacement therapies (like patches and gums). But one area of study where research may be lacking is with regard to long-term use.
The source of rampant misconceptions about nicotine is likely due to decades of campaigning from anti-tobacco groups that treat all tobacco and nicotine products as if they are equally harmful, compared to cigarettes. Misunderstandings about nicotine are detailed in the results of a 2019 Rutgers survey showing that more than 80% of doctors mistakenly believe that nicotine contributes to cancer, heart disease, and COPD. A 2018 study also reveals that more than half of adults in the US mistakenly think nicotine causes cancer.
The byproducts of burning tobacco leaf are what contribute to smoking-related diseases, not nicotine.
Epidemiological studies of nicotine replacement therapies (patches, gums, lozenges) and Swedish snus (a form of smokeless tobacco) have shown that nicotine consumption – outside of smoking cigarettes – does not increase a person’s risk of developing any of the previously mentioned diseases more than the rates observed in people who don’t use nicotine. Consuming nicotine is not completely risk-free, but the health benefits of quitting smoking far exceed the risks.
Nicotine is also being studied for its potential therapeutic and preventative effects in diseases like Ulcerative Colitis, Parkinson’s, Alzheimer’s, ADHD, schizophrenia, dyskinesia and even COVID-19.
addiction
When people use the word “addiction,” they are typically referring to some kind of habitual behavior that negatively affects someone’s health, well-being, and ability to function in life. As addiction science has evolved, many in the field are recognizing that certain words are stigmatizing and have a history of being used to shame people into changing their behavior. A practice that was once regarded as necessary in order to motivate people who smoke to make attempts to quit, is gradually being exposed as a tactic that marginalizes and “others” people in ways that actually discourage them from seeking support.
Safer nicotine products do not immediately fall into the category of “addictive.” The more accurate description would be “dependence,” or “habit-forming,” which typically means someone is physically or mentally reliant on a product – but it’s not negatively affecting their life. Many people would admit to being dependent on caffeine, but we wouldn’t call it an addiction because coffee doesn’t ruin lives, break up families, cause financial problems, or pose a threat to health at a population level.
People using safer nicotine products may be dependent on nicotine, but it’s typically no more problematic than needing that first cup of coffee in the morning.
Lee, P. N., & Fariss, M. W. (2017). A systematic review of possible serious adverse health effects of nicotine replacement therapy. Archives of toxicology, 91(4), 1565–1594.
McDonald, J. (2020, September 17). More Than 80% of Doctors Think Nicotine Causes Cancer. Vaping360.
McDonald, J. (2018, March 9). Americans Mistakenly Believe Nicotine Causes Cancer. Vaping360.
Pullan, R. D., Rhodes, J., Ganesh, S., Mani, V., Morris, J. S., Williams, G. T., Newcombe, R. G., Russell, M., Feyerabend, C., Thomas, G., & Sawe, U. (1994, March 24). Transdermal Nicotine for Active Ulcerative Colitis. The New England Journal of Medicine. 10.1056/NEJM199403243301202
Hurley, D. (2014, February 4). Nicotine, the Wonder Drug? Discover Magazine.
Val, E. (2020, April 22). French study shows nicotine could protect against Covid-19. La Vanguardia.
lgbtq community
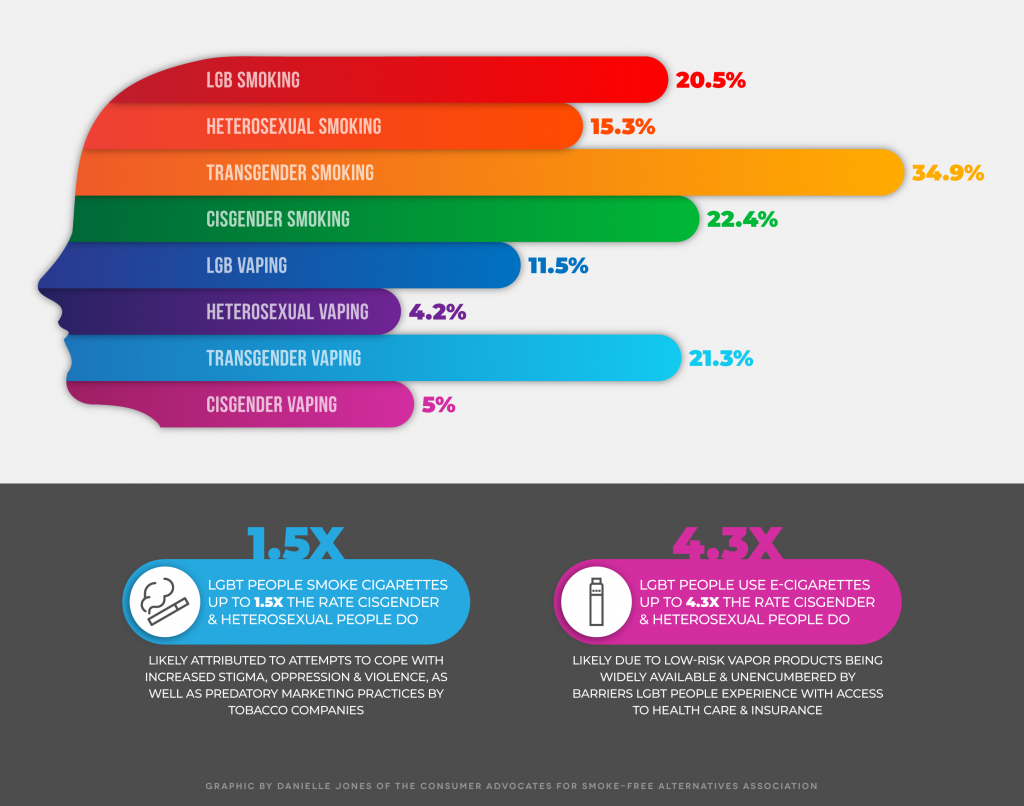
CASAA is dedicated to providing truthful and complete information to consumers about low-risk alternatives to smoking so that they can make informed choices. Certain underrepresented populations continue to be affected by disproportionately higher smoking rates, as well as early death and disease attributed to smoking. One of the hardest hit populations continues to be the LGBTQ community. With over 30,000 early deaths per year attributed to smoking, the percentage is astonishingly higher than that of people who identify as heterosexual.
Data from the 2019 National Health Interview Survey reveals that LGB adults smoke cigarettes at 1.4x the rate that heterosexual individuals do (19.2% versus 13.8% respectively), and while data on transgender adults is limited, a study from 2013 shows that trans individuals smoke at 1.7x the rate cisgender adults do (35.5% and 20.7% respectively).
A recent U.S. study reported that lesbian teenagers are twice as likely to smoke as heterosexual teenage girls. We also know that the reported 30,000 LGBTQ people who die each year from illnesses attributed to smoking is more than double the number of deaths from HIV/AIDS, which are reported at 12,000 per year.
Why are smoking rates so much higher in certain communities?
- Stigma
- Stress
- Depression
- Trauma
- Alienation
- Social bonding/Fitting in
- Poor information about
safer products
Harm reduction is a set of practical strategies and ideas aimed at reducing negative consequences associated with drug use. Harm reduction is also a movement for social justice built on a belief in, and a respect for, the rights of people who use drugs.” – Harm Reduction Coalition
At the height of the HIV/AIDS epidemic in the ‘80s and early ‘90s, more than 50,000 people were dying each year from AIDS-related complications. Public health crises were declared, and we saw the implementation of public information campaigns, needle exchanges, and free condoms with such success that we now see a sharp decline to approximately 12,000 deaths annually. This is one example of harm reduction at work.
how is harm reduction related to smoking?
It accepts that the motivation to chemically alter our mood is part of our world and chooses to work to minimize its harmful effects rather than simply condemn or ban the behavior. It understands tobacco use is a complex, multifaceted phenomenon (especially for the LGBTQ community) that encompasses a continuum of behaviors and acknowledges that some ways of consuming nicotine-containing products are clearly safer than others.
It calls for non-judgmental, non-coercive provision of services and resources to people who use nicotine to assist them in reducing health risks if they choose to do so. It ensures that tobacco and nicotine consumers have a legitimate voice in the creation of programs and policies designed to serve them. It affirms tobacco users themselves as the primary agents of protecting their health and seeks to empower the people to share information and support each other. It recognizes that the reality of poverty, class, racism, social isolation, past trauma, sex-based discrimination, and other social inequalities affect both people’s vulnerability to, and capacity for, effectively dealing with decisions related to tobacco and nicotine use.
It does not attempt to minimize or ignore the relative risk and potential for harm associated with tobacco use. It emphasizes the quality of individual, community life, and well-being–not necessarily nicotine cessation–as the criteria for successful interventions and policies.
LGBTQ Adults Are Already Embracing Tobacco Harm Reduction
Nationally representative surveys tell us that the LGBTQ community is already embracing reduced-harm vapor products faster than heterosexual and cisgender adults. LGB individuals use electronic cigarettes at 2.7x the rate heterosexual adults do (survey data was limited to lesbian, gay, and bisexual adults), and transgender adults vape at an astounding 4.3x the rate cisgender adults do.
These use rates show the dramatic live-saving potential of safer nicotine products within the LGBTQ community, likely because vapor products have been widely available and unencumbered by barriers LGBTQ people experience with access to health care and insurance.
Solutions should empower communities to act on their own behalf
CASAA is providing the following information media to enable discussion of smoke-free alternatives within the LGBTQ community:
This video explains the important difference between smoking and vaping, as well as the implications for using vaping as a tool to dramatically reduce smoking related harms
A summary that covers a range of issues including the case for tobacco harm reduction, exposure risks for e-cigarette users, and policy recommendations from Clive Bates
A report commissioned by Public Health England was the first major health agency in the world to conclude there is overwhelming evidence that using e-cigarettes is dramatically less risky than smoking
RCP is the oldest medical college in England. Their report in 1962 outlined the considerable dangers of cigarette smoking two years ahead of the US. With this report they outline the evidence and assert the “huge potential” of e-cigarettes to prevent smoking related death

We Can't Do It Without Your Support
We rely on donations from generous supporters like you.
Every little bit helps!

